
Physiotherapy Treatment of Cervical Spondylosis
Cervical spondylosis is one of the most common conditions referred by doctors to physiotherapists. In this article, we discuss the several causes of pain in cervical spondylosis and the anatomical structures responsible for it. We will cover specific treatment targeted to each of these structures. This highlights the crux of our clinical reasoning, and adds clarity on how the actual cause is treated. This makes the recovery lasting and more cost-effective for patients (Jull et al 2002, ).
The basic assessment for patients with cervical spondylosis starts with a posture check. This specifically identifies and treats the affected joints and muscles. A brief summary follows below:
Posture
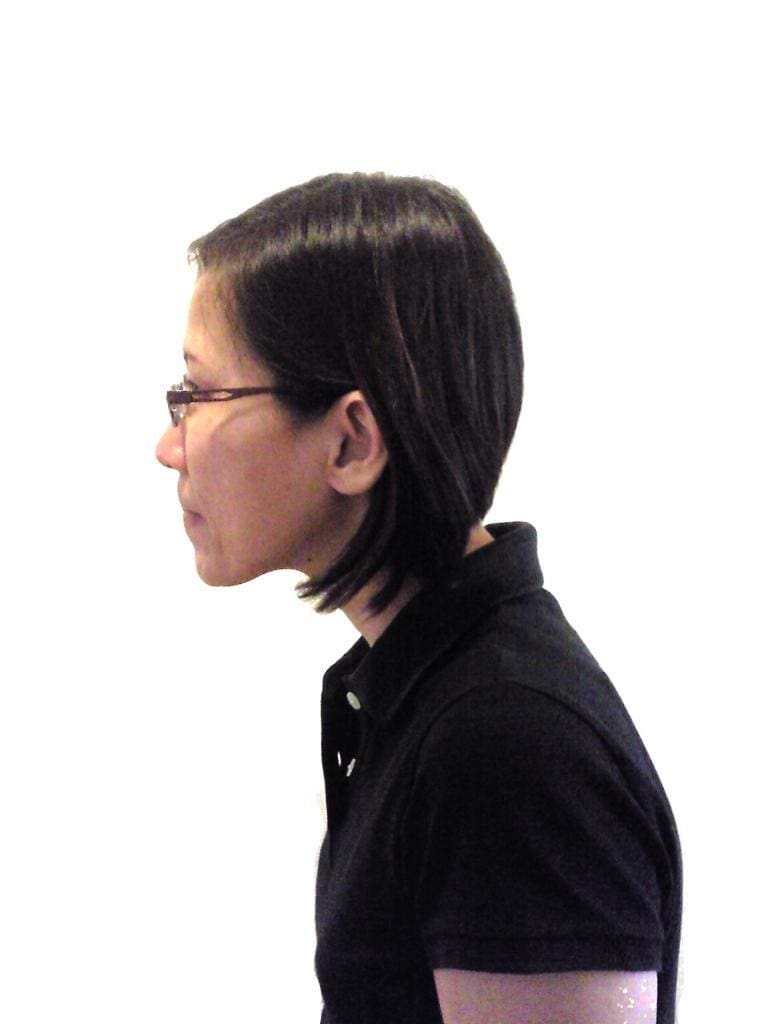
Often, patients with neck pain present with a forward head posture (see fig 1), thoracic kyphosis and either a lordotic or flat lower back. The lower cervical is in constant flexion. On the other hand, their upper cervical is in extension. This is due to the thoracic kyphosis. This posture will put the C0/1, C1/2 and maybe C2/3 facet joints in constant compression, leading to joint degeneration at those levels. Pfaffenrath and Kaube (1990) and Nilsson (1995) found that 14-18% of chronic headaches are cervicogenic, i.e. headaches. These resulted from musculoskeletal dysfunction in the cervical spine. Hence we assess and treat the upper cervical spine in patients with cervicogenic headache. Any treatment will be short term. This is so, unless the compression on C0-3 is relieved through thoracic spine extension and upper cervical retraction.
Joints

Due to the facet joint degeneration in cervical spondylosis, the affected joints will have a loss of normal range of movement. This results in other levels having to compensate, leading to increased loading and eventual wear and tear. The general range of motion is limited. Clients too tend to complain of achiness (“sng”) in the neck and referred pain to the respective dermatomes when there is significant amount of hypomobility. Zito et al (2006) found that in cervicogenic headaches C0/C1, C1/2 were significantly hypomobile. Hypomobility is treated with mobilization of the affected facet joints and self-mobilization techniques using a Mulligan cervical strap.
Another presentation that we as physiotherapists find is that the vertebrae can be rotated either at one level or at several levels. This happens when there is muscle spasm, trigger points or hypertonic muscles unilaterally at those levels causing lateral flexion. Since those joints are already malpositioned, it is impossible to have a normal range of motion at those levels. Using those joints in our functional activities which require full range will result in irritation of the surrounding structures. To normalize range requires normalization of the position of the vertebrae. This is done by reducing spasm and lengthening the affected muscles. A technique that is often used to achieve this is called Muscle energy technique (see fig 2). This technique involves submaximal contraction of the affected muscle and on post contraction, this muscle in stretched to a new length. This is a more effective technique than plain stretching because of the specificity of the level and enhanced post contraction- relaxation phase. Muscle energy technique promotes muscle relaxation by activating the golgi tendon reflex. It has also been proposed that temporary muscle fatigue blocks reflex-contraction thus allowing for an increase of range of motion to beyond the barrier.
Muscles
Wrong types of muscles are sometimes used. This imposes undue stress on the spine and causing pain due to poor posture. There are two basic types of muscle – phasic (power muscles) and tonic (postural muscles). The power muscles create movement. Examples of these muscles in the neck are the sternocleidomastoid (SCM), scalenes and the levator scapulae. The tonic muscle work at low levels and their function is to stabilize. Examples of such muscles in the neck are the deep neck flexors and the longus capitus and colli.

When the head is held in a forward head posture, the deep neck flexors (which are in front of the neck) are lengthened and weak. The role of stabilisation of the cervical spine is now compensated by the phasic muscles. As these muscles are not designed to contract for prolonged periods of time as required for stabilization, they tighten and develop overuse trigger points. The trigger points themselves can be painful and may refer elsewhere.
Clinical Studies
In a study (Zito et al 2006) that looked at neck pain and cervicogenic headache, it was found that the incidence of muscle tightness was significantly higher in the power muscles such as the upper trapezius, levator scapulae, scalenes and suboccipital extensors when compared to control and migraine sufferers. EMG activity for SCM was also higher when neck pain and headache sufferers were asked to perform a craniocervical flexion test. This indicates an altered pattern in the neck flexor synergy where there is a poor contractile capacity of the deep neck flexors which are suited for craniocervical flexion. Treatment requires retraining of the tonic deep neck flexors (see fig 3) and release of the muscle tightness in the phasic muscles.
In a study, Jull et al (2002) compared the effectiveness of manual therapy alone to a group that received both manual therapy and deep neck flexor exercise to a control group. Significantly lower intensity and frequency of pain were found in groups that received either manual therapy alone or both manual therapy and exercise therapy as compared to controls. Interestingly, when the groups were reviewed 12 months later the group that received a combination of exercise and manual therapy did much better than the other groups. This suggests that a specific exercise program yields a better outcome over the long term.
These results reinforce the clinical evidence that the deep cervical flexors are important muscles for cervical segmental and postural control and lose their endurance capacity in patients with neck pain (Watson and Trott 1993).
Cervical spondylosis treatment
A review of the above literature and clinical findings brings us to the conclusion that definite dysfunctions exist in patients with neck pain and cervicogenic headache. Changing the symptoms with electrotherapeutic modalities only looks at the tip of the iceberg. Treating the dysfunctions of cervical spondylosis in posture, joints and the muscles not only resolves the neck pain and headache solves the cause reducing future incidents.
References:
- Jull G, Trott P, Potter H, Zito G, Shirley D, Emberson J, Marschner I and Richardson C. (2002) A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 27 (17): 1835-1843
- Nilsson N. (1995) The prevalence of cervicogenic headache in random population sample of 20-59 year olds. Spine 20:1884-8
- Pfaffenrath V and Kaube H.(1990) Diagnostics of cervicogenic headache. Functional Neurology 5:159-64
- Watson DH and Trott PH (1993) Cervical headache. An investigation of natural head posture and upper cervical flexor muscle performance. Cephalagia13:272-284
- Zito G, Jull G and Story I (2006) Clinical tests of musculoskeletal dysfunction in the diagnosis
- Lewis, M., James, M., Stokes, E., Hill, J., Sim, J., Hay, E., & Dziedzic, K. 2007, “An economic evaluation of three physiotherapy treatments for non-specific neck disorders alongside a randomized trial”, Rheumatology. (Oxford), vol. 46, no. 11, pp. 1701-1708
Related Articles
- Top 3 posture types leading to back pain You’ve tried pilates and yoga, ergonomic back supports, and back braces, but your chronic back pain persists. So what is…
- Basketball Injuries - 3 Common Injuries & How… Basketball has gained popularity around the globe since its creation 100+ years ago. With a standard hoop located 3+ metres…
- Coping With Pregnancy Related Musculoskeletal Discomforts The majority of musculoskeletal problems that arise during pregnancy can be prevented and treated with physiotherapy intervention. Individualized physical therapy…
- Exercise therapy: Coping with pregnancy related discomforts Most of the musculoskeletal problems that arise during pregnancy can be prevented and treated by physiotherapy. Individualized physical therapy programs…
- Common Cycling Injuries in Singapore: What They Are… Cycling is a fantastic sport and offers a plethora of benefits. Unfortunately, it can also result in a number of…

